Real-World Type 1 Diabetes—Getting An Insulin Pump: Misconceptions vs. Realities
I was really…irrationally…scared of the idea of getting an insulin pump
When I was diagnosed with type 1 diabetes at age 42…near the beginning of the COVID pandemic…the year after I sold my house and most of my belongings to live nomadically…you could say I was a bit overwhelmed. A nomadic lifestyle I was learning while doing—I had only seen my 3rd country outside the US two years earlier—was now forced into a new lifestyle that I definitely didn’t understand.
Even though I picked up my understanding of how to manage my type 1 diabetes pretty quickly, I was honestly scared to death at the idea of getting an insulin pump as opposed to managing with multiple daily injections (MDI) and insulin flexpens.
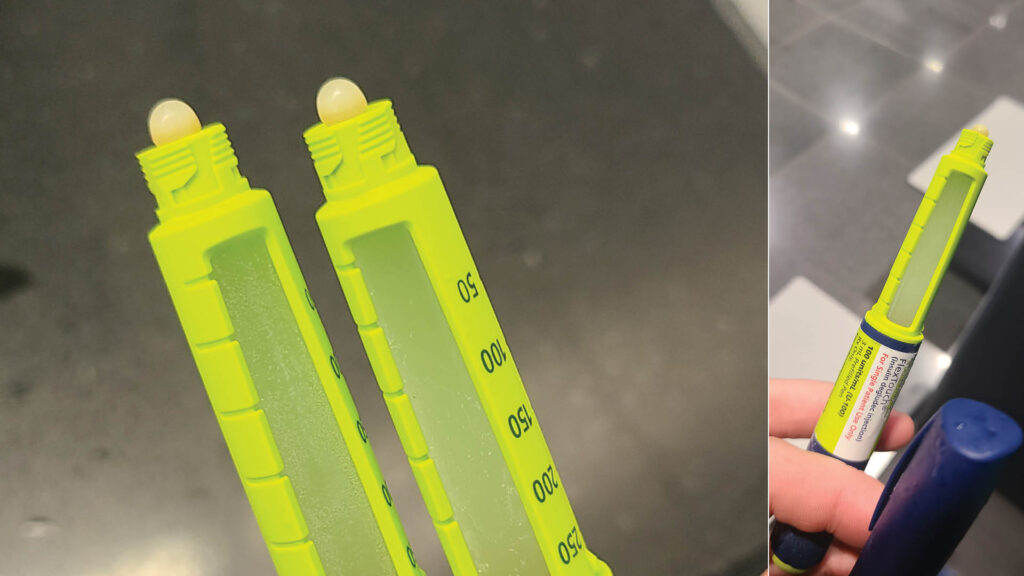
From the moment I was diagnosed, managing MDI with Novolog (insulin aspart rapid-acting insulin) for mealtime boluses and Tresiba (Insulin degludec) long-acting basal insulin—accompanied by a Freestyle Libre 2 glucose monitor—was all I knew.
I’ve always been really thankful for how I was able to manage those early days with multiple daily injections, but I had no idea how my life would change once I eventually chose to get an insulin pump.
The thing is…you don’t know what you don’t know…or try. So at that time, other than the expensive financial realities of an insulin pump, the biggest thing holding me back was fear and ignorance.
And as a person that literally encourages others to experiment with life instead of leaving things to thought or conjecture…eventually I had to listen to my own advice.
This site participates in the Amazon Services LLC Associates Program and other affiliate programs and may earn from qualifying purchases. You’re never charged more, but it helps out little by little! Check out “Privacy” in the top menu if you need to know more!
Disclaimer: This diabetes blog is based on my personal journey managing type 1 diabetes. Everyone's type 1 diabetes journey is unique, and what works for me might not work for your situation. I'm not a medical pro, The info here isn't a substitute for professional medical advice, diagnosis, or treatment. Talk with your doctor before making any decisions regarding your diabetes care. - Jason
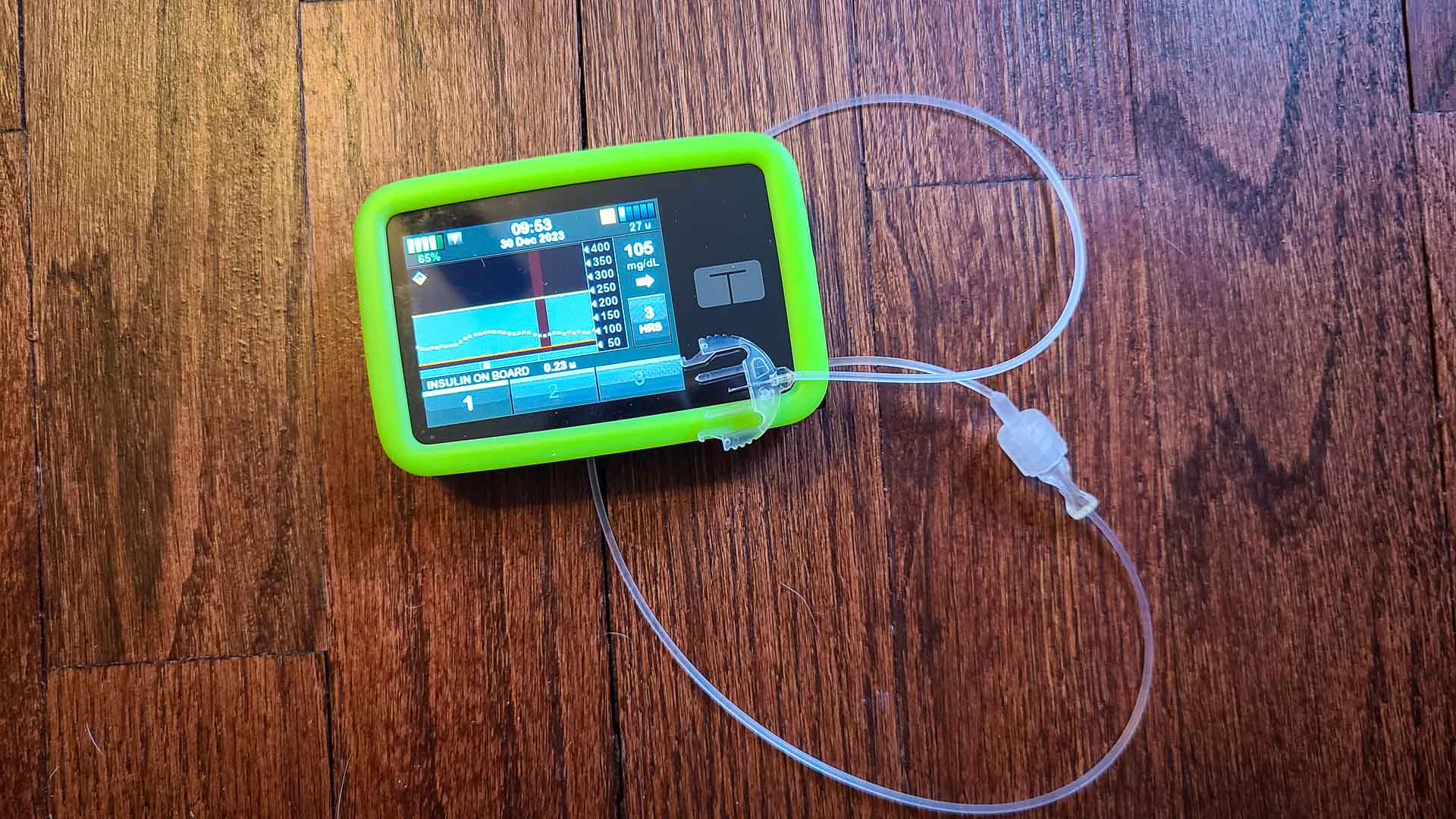
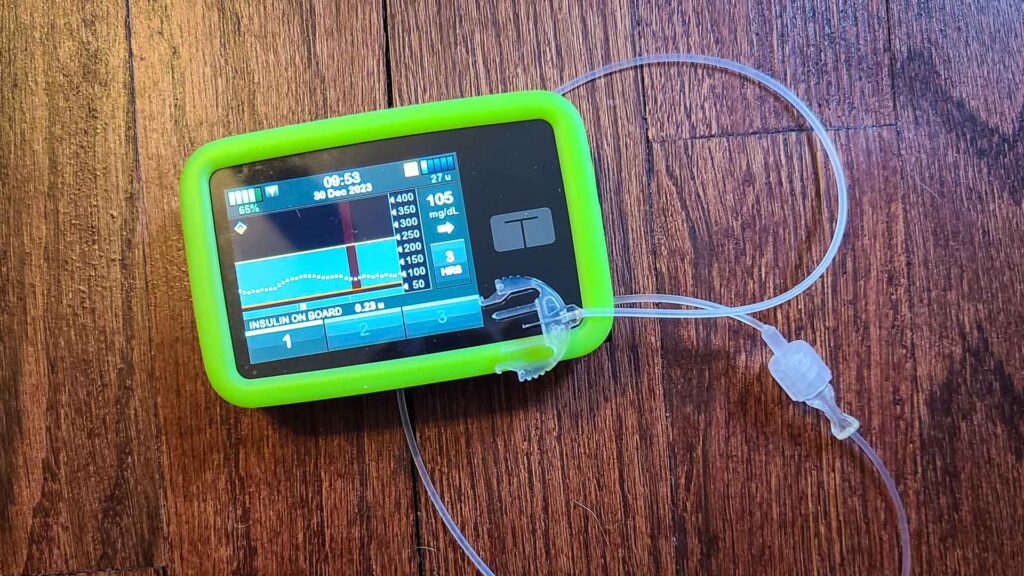
How I currently manage my type 1 diabetes: Tandem insulin pump connected to a Dexcom continuous glucose monitor
As of this writing I manage my type 1 diabetes with Dexcom G6 or Dexcom G7 continuous glucose monitors and for insulin delivery use a Tandem t:slim X2 insulin pump and Novolog insulin aspart.

Of course, I still carry insulin flexpens with me in case the pump fails, but I’ve been pretty much insulin pump dependent since the day I got it (after a year of MDI), other than a couple very interesting pump breaks.
Oh…and this article isn’t sponsored…but a boy can dream. This is all real, based on my experiences.
Connect & Share This Article
True & False—how this article is set up
Essentially, I want to tell you exactly all of the things that I had wrong…or right…about insulin pump life so that you have a real world take on it. Maybe you’re thinking about getting an insulin pump for your diabetes care and you’re doing your research.
Or maybe you’re on one and thinking about another, or just looking to see how others manage on an insulin pump. Regardless, hopefully you find something helpful here, for you or someone you’ll share this with.
Each section will have a headline assumption that I had, then some true and false—purely based on my own experiences—and then some parting thoughts. Not right, not wrong, just my experience and thoughts, so please be kind. Some of these things might seem a bit off the wall, but they’re all based on feelings and emotions I worked through…or still work through…while managing my type 1 diabetes with an insulin pump.
READ NEXT: Gifts For Diabetic Travelers—Essential Travel Items & Unexpected Gifts
I Just Got Diagnosed With Diabetes And I’m FREAKING OUT!
Using an insulin pump to deliver insulin won’t improve my life that much
Big, huge, giant, loud-yell…false. Yep, I’m coming out of the gates with probably the strongest spoiler alert I can. But it’s probably the biggest most important reality of all of what will follow here. My insulin pump has completely changed the game on my type 1 diabetes management, and my life is so much better for it.
From the relatively “simple” real-time reasons like background automatic correction boluses or increases and decreases in basal insulin, to sport or sleeping mode benefits, to the longer-term improvements to A1C and time in range, it adds up.

The insulin pump does all the work
Somewhat true…but is that a good thing? An insulin pump, especially one of the current ones on the market, does a ton of the work for you, often in the background, but that’s a double edged sword. The bad part about it is that it can make you pretty complacent and kind of “forget” how to manage your diabetes without a mini computer doing most things for you.
Note that for an insulin pump to do more work for you it will likely need to “talk” to your continuous glucose monitor.
I suggest actually taking an insulin pump break every once and a while and going back to insulin flexpens and multiple daily injections for insulin delivery for at least two reasons. One, it forces you to remember how to manage with MDI and how much insulin you need, which you need to know in case your your pump stops working or gets broken, lost, or stolen.
And reason two…it’s really humbling and actually makes you appreciate and have gratitude for being fortunate enough to have a pump.
The false part. You still need to understand the amount of carbs in whatever you’re eating and actually administer an insulin bolus at mealtime. With a pump you also have schedules for sleep, or the ability to switch into a sport or temporary mode, all of which require some brain power and awareness.
And when life throws you curves like sickness, or major changes in routines, it’s likely you’ll want to adjust the settings or have multiple settings to be able to switch to.
Finger pricks and insulin delivery by flexpens gets old quickly
Also, very few diabetics I’ve met like the idea of stabbing ourselves more than necessary, so an insulin site change every 2-3 days as opposed to 6-10+ flexpen pokes a day for insulin delivery is great.
Beyond all of those (and more) reasons, there are also the emotional and mental improvements that come along with them.
Yes, I can attest that the overwhelm of the swings in blood glucose level highs and lows with MDI results in a lot of mood swings, and that using an insulin pump that has some cruise control benefits can really help smooth things out a bit.
Insulin pumps are confusing
True and false. This is where the balance of your personal level of detail and desire to learn compared to your interest in setting it and forgetting it come in. My endocrinologist has repeatedly told me that my grasp of type 1 diabetes, management methods, and my pump understanding is really high compared to a lot of his other patients.
So for me, a very…overly analytical and detail oriented person, it’s not too confusing, and I kind of nerd out on it all.
For someone that doesn’t use a lot of tech or is more of a passive person as it comes to the details, figuring out how to program the pump could be a little bit confusing.
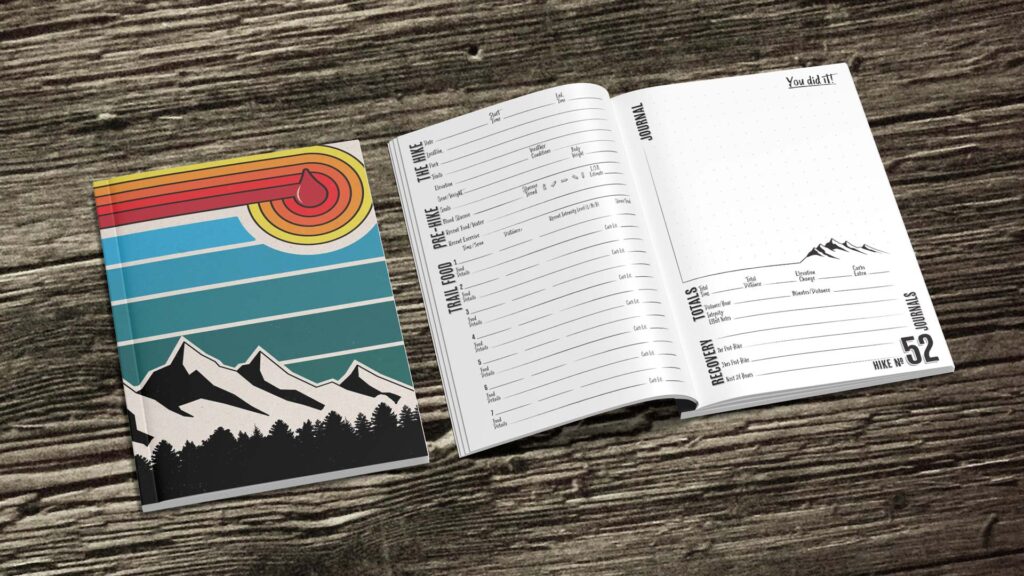
READ NEXT: Tips For Hiking With Type 1 Diabetes – From A Type 1
Tips On How To Use An Emergency Hiking Whistle…And Why You Should Have One
But honestly, managing type 1 diabetes with an insulin pump connected to a CGM, with all of that data being compiled and accessible, can allow you to be much more passive and plan most of the changes or adjustments to to be handled during your visits with your endocrinologist. So if that’s your jam, go for it.
People will judge me because I have a mini-computer & tubes plugged in all the time
Mostly false. Most of the time, if it comes up, any conversations about my insulin pump quickly turn to the fact that this little super computer literally keeps my life on track…and keeps me alive, if you want to be dramatic.
Curiousness about my insulin pump and what I’m doing at mealtime often turns into a welcome Q&A where I get to give some knowledge and the other person gets to become a little more sympathetic. They get to learn about how my pump therapy works, as well as what life with type 1 looks like.
A little bit true. I wouldn’t classify it as judgement really, but more true ignorance and statements made out of that—which are quickly retracted or realized once the person knows what my insulin pump does for my life. So the somewhat annoying “Dude…is that a Tamagotchi?” questions (Tamagotchi were digital “pets” back in the 90s) do get old, but they’re harmless.
Connect & Share This Article
My intimate life will be ruined if I have an insulin pump
Mostly false. I used to worry, especially since I was single when diagnosed, that anyone I met and dated would really have a hangup about my choosing to wear an insulin pump. I worried that sex and spontaneity or even just the intimacy at all would be really impacted by it, or that having robot parts on my body would be a total downer. All of these for the most part have proven a non-issue.
While everyone manages differently, I have no issue unplugging for a while when needed. Showers, water adventures, just a break when I know my numbers are good for a while…or for sex and shenanigans.
Assuming my blood glucose numbers are fairly flat…it’s usually not a huge deal. And a good partner can even making it part of foreplay by giving a mischievous look, asking how my numbers are, and motioning/asking if I can unplug for a while. (Brown chicken brown cow…)
A little true. I’d be lying if I said it was all roses. Always having diabetes robot parts to bump into…or get ripped out…can suck. And it definitely happens. And when things are moving quickly and clothes are flying, it sucks to pause and make sure blood glucose levels are sorted…but that would need done if on flexpens too, so it’s really not something that would be avoided, just different methods.
READ NEXT: Gifts For Diabetic Travelers—Essential Travel Items & Unexpected Gifts
Sleeping with an insulin pump will be annoying
Well, kind of true. If you’re getting your insulin delivery from a pump, you’ll likely have to wear that pump the majority of the 24 hours in a day to get the full benefit of it. Because many current pumps on the market deliver continuous background doses of basal insulin, it’s necessary.
The misconception I had was that I would constantly be ripping out my infusion set or it would be uncomfortable, or my literal insulin pump would get in the way all the time. Just not true.
After a few weeks, my “sleep brain” just got used to it and would grab, move, adjust, or organize my pump as I moved in the middle of the night without me even really thinking about it or it obstructing my routine.
When sleeping with an insulin pump, many people it a pocket or wear special clothing with pump pockets. But I sleep…um…au naturale, so my pump just lay on the bed beside me. If I move, I grab, roll, drop, no worries. And honestly, I’ve probably only pulled out less than a handful of sites in the two years since I got my pump.
But…it is annoying to be connected. If my blood glucose numbers are really in order, and considering a flatline going to bed means your body isn’t using much stored glucose, sometimes I’ll just take a break for a few hours. It’s all up to the situation.
Pump life has a lot of waste…and baggage…and makes long-term travel hard
True…insulin pump life has soooooo much waste. For my Tandem t:slim X2 insulin pump, I change cartridges every 2-3 days, which includes infusion set and tubing, a syringe for filling. That is just a ton of waste, with no real way around it.
Luckily companies are making pumps and their supplies smaller and smaller, but all in due time. Also, since I use Dexcom continuous glucose monitors, those are also adding to the waste.
And it’s so much more to pack for any trip, let alone for a person like me that used to travel carry-on only.
Packing for travel—plan for lots of space for insulin pump gear
If you’re only going for a week or two, it’s probably not a big deal. But I am often international for 2-3 months, so add in “emergency supplies” and extras in case things go wrong, and I’m adding literally more than 1-1.5 square feet of medical supplies to my packing game.
And all of my insulin pump and diabetes supplies and insulin has to go carry-on in the plane cabin with me. I can’t chance losing literally thousands of dollars worth of supplies, let alone figuring out how to replace them in some far off destination.
Read Next:
I Froze My Insulin Flexpens—Tips For Traveling With Insulin Internationally
Diabetes Symptoms For Noobs – My Type 1 Diabetes Symptoms & Diagnosis Story
Having an insulin infusion set connected with a needle in my body at all times will be painful
Mostly false. Let me say first that this likely has a lot to do with two things: your body style (amount of fat to be able to put your needle), and your infusion set choices.
I’m pretty skinny, so even with my very short metal infusion set needles (I use Trusteel metal 6mm cannula sets with a 23” tube) I still feel some pain when I move wrong or tense and the needle hits past the fatty parts of my sides.
And I’ve completely gone away from plastic cannula sets as my experience has been really bad with those from the standpoints of pain or occlusions (bends or blocks in the cannula).
Connect & Share This Article

Managing type 1 diabetes with an insulin pump is really expensive
Very True. Sorry to be a bummer, but for the most part, this one is a reality. And I’m super grateful to be in a position to be able to afford my pump and yearly costs, and really wish everyone that wanted one could. But this ish is expensive.
The insulin pumps alone can cost thousands without insurance, so playing the “met deductable” card and getting one when it’s mostly covered is almost mandatory. Or you can check for insulin pump financial assistance programs if insurance isn’t helpful.
But the cost of the pump is just the beginning—I swear these companies make all their money off of the supplies we need to actually use our insulin pumps.
Currently my out of pocket costs just for insulin pump cartridges, infusion sets, and Dexcom continuous monitors is about $300/month after insurance. So upwards of $4000 a year out of pocket.
That doesn’t include insurance premium costs or insulin costs, or any of the costs for other prescriptions. Of course, all of this can vary wildly based on insurances, but the bottom line is that it costs more to manage type 1 diabetes on an insulin pump.
But for the most part I feel very little pain on insertion anymore, and when I’m putting my infusion set on a part of my body with a little fatty tissue, it’s relatively painless while wearing, the majority of the time.
If you can afford the pump and the ongoing costs, I highly recommend getting an insulin pump
As of this writing, of the roughly 37 million US citizens that have either type 1 or type 2 diabetes, only about 350,000 use an insulin pump, and I’m sure the majority of those folks are managing type 1 diabetes. That’s a pretty small percentage of people, given the amazing health and quality of life improvements using a pump has shown in studies.
Unfortunately at the end of the day a lot of our type 1 diabetes management decisions come down to money. The percentage of my income that goes towards my health management is nauseating, so I get it.
If you can afford it—not just getting the pump, but the ongoing costs—the benefits to your long term health as well as your mental and emotional health will likely be worth going for it. If you’re not sure, just start asking a lot of questions.
Talk to your Endocrinologist about their recommendations for different pumps on the market, talk to your health insurance about what might or might not be covered and run some numbers, and call pump manufacturers and ask them questions. Make sure you ask about financial assistance programs of all of these sources.
Hope this article helped! Sharing is caring!
Cheers!

About Jason Robinson
Jason is the author of “The Beginner Traveler’s Guide To Going Nomad,” as well as the voice behind the words and the eye behind the lens for The Nomad Experiment. “Planning to travel at some point” wasn’t actually getting the job done, so nearing 40 he decided to make it a priority, nomatter how scary that was. A few years later—through the pandemic and a type 1 diabetes diagnosis at age 42—now living a life of nomadic travel, he’s speaking out to encourage others of any age, or with any serious medical diagnosis, to live an unconventional life.
PS – You can check out more products recommended for long-term travel and daily life with diabetes here.
RELATED ARTICLES:
Gifts For Diabetic Travelers—Essential Travel Items & Unexpected Gifts
I Froze My Insulin Flexpens—Tips For Traveling With Insulin Internationally
I Just Got Diagnosed With Diabetes And I’m FREAKING OUT!
Diabetes Symptoms For Noobs – My Type 1 Diabetes Symptoms & Diagnosis Story
Connect & Share This Article